ARTICLE AD
A new approach to Alzheimer's disease treatment could be on the horizon, inspired by a compound found in common herbs.
Carnosic acid is found in rosemary and sage and is known for its antioxidant and anti-inflammatory properties; however, it is unstable in its pure form.
Now researchers in California have synthesized a stable derivative of the compound, which showed promising results in mouse models of Alzheimer's.
Mice that were given the stable derivative had boosts in memory, more neuron synapses, reduced inflammation, and more removal of toxic proteins that are linked to Alzheimer's.
That covers multiple signs of Alzheimer's disease, which can kill off a high proportion of synapses, breaking key neuron communication routes, while memory loss is one of the most noticeable effects.
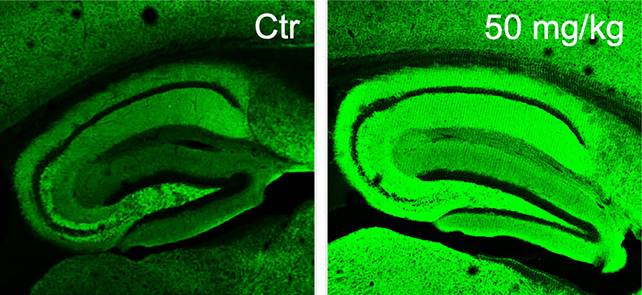 Microscopy images showing an Alzheimer's-like mouse brain (left), and a diAcCA-treated mouse brain (right), with more intense green colors showing more neuronal synapses. (Scripps Research)
Microscopy images showing an Alzheimer's-like mouse brain (left), and a diAcCA-treated mouse brain (right), with more intense green colors showing more neuronal synapses. (Scripps Research)"We did multiple different tests of memory, and they were all improved with the drug," says neuroscientist Stuart Lipton, from the Scripps Research Institute.
"It didn't just slow down the decline, it improved virtually back to normal."
One of the main challenges faced by the researchers was getting carnosic acid into a stable form that would last long enough in the brain to have an effect. After extensive tests, they found a suitable di-acetylated form (diAcCA).
The gut converts diAcCA to carnosic acid before it enters the bloodstream, where they found it has about 20 percent better absorption than pure carnosic acid. Once converted, the carnosic acid reached therapeutic levels in the brain within an hour.
Mice with a form of Alzheimer's were then given diAcCA or a placebo three times a week for three months. The researchers looked at the effects on brain tissue and how well the mice did on exercises designed to assess their memory and ability to learn.
The diAcCA compound didn't appear to have any toxic effects on the mice treated with it, and excessive buildups of proteins known to be signs of Alzheimer's damage were reduced in their brains.
"By combating inflammation and oxidative stress with this diAcCA compound, we actually increased the number of synapses in the brain," says Lipton.
"We also took down other misfolded or aggregated proteins such as phosphorylated tau and amyloid beta, which are thought to trigger Alzheimer's disease and serve as biomarkers of the disease process."
It's all very promising, although we're still at the early stages here. Clinical trials will be needed to confirm that diAcCA has the same effects in human brains.
Given the anti-inflammatory properties of carnosic acid, which have also been recorded in previous studies, Lipton and his colleagues are hopeful that this same treatment could be used for other conditions linked to inflammation – from type 2 diabetes to Parkinson's.
There's also potential for diAcCA drugs to be used alongside other treatments for Alzheimer's that are now available. As this compound is a modified form of carnosic acid – already known to be safe for consumption – the researchers are hoping new medications can be developed on an accelerated schedule.
"It could make existing amyloid antibody treatments work better by taking away or limiting their side effects," says Lipton.
The research has been published in Antioxidants.

 4 hours ago
1
4 hours ago
1 

