ARTICLE AD
Scientists in Australia think they have discovered a better way to treat the deadliest and most aggressive form of breast cancer.
Unlike chemotherapy, the new treatment approach kills and slows the growth of only cancerous cells within breast tissue, not normal, healthy ones.
The oral medicine also targets metastatic lesions that have spread elsewhere in the body and show resistance to chemotherapy.
Triple-negative breast cancer accounts for up to 15 percent of all breast cancers, and it is notorious for growing and spreading relatively fast, even among young patients.
To date, there are no targeted drug treatments available to combat this form of cancer, leaving patients with only a few broad options: intensive chemotherapy or cutting-edge immunotherapy. Even then, the chances of relapse within five years are high.
If the cancer spreads to distant locations outside localized breast tissue, the five-year survival rate can fall from 91 percent to 12 percent.
New forms of treatment are desperately needed to save lives.
"This is an exciting development in the battle against triple negative breast cancer," says breast cancer expert Theresa Hickey from the University of Adelaide, who led experiments on the new oral medicine.
"The results of this study show that this drug could hold the key to improving survival rates."
The drug in question is called CDDD11-8, and it was initially developed to treat acute myeloid leukemia (AML).
AML is a cancer that grows in bone marrow, and it is difficult to target. The cancerous cells survive, grow, and spread by ramping up protein production, especially via a pathway called cyclin-dependent kinase 9 (CDK9).
To date, the United States Food and Drug Advisory has not approved any drug that inhibits CDK9, though one version has shown initial clinical benefits.
In 2022, researchers at the University of South Australia developed CDDD11-8 to selectively inhibit CDK9. When tested on animal models, the oral drug triggered "robust tumor growth inhibition" that "translated to an improved survival of animals" with leukemia.
Now, that same drug shows promise in treating triple-negative breast cancers, too.
"It is still early days but based on this initial evidence, we believe inhibiting this protein could lead to a treatment for triple negative breast cancer and this new drug should be developed further," says Hickey.
She and her team at the University of Adelaide think that targeting CDK9 could also work for other aggressive cancers that are "addicted to transcription".
Transcription is the copying of genetic instructions into RNA molecules, which then help control protein production.
In cancerous cells, transcription is often 'out-of-control' compared to healthy cells. This helps the disease rapidly grow and spread, leading to worse outcomes for patients.
Triple-negative breast cancer is a cancer with a particularly high abundance of transcription factors, so which one should scientists try to shut down?
The CDK9 pathway could be a useful target because it is one that normal, healthy cells don't seem to rely on for survival nearly as much as aggressive cancerous cells.
Hickey and her colleagues think CDDD11-8 should now be clinically evaluated for the most aggressive type of breast cancer.
In initial experiments, when this novel drug was administered to cell-line models of triple-negative breast cancer, researchers noticed a reduction in cancer growth and an increase in cancer cell death with varying degrees of success depending on the dosage.
The drug also showed promise in living mouse models with breast cancer. Mice treated with oral medicine showed shrunken tumors and reduced protein expression without adverse effects on vital organs.
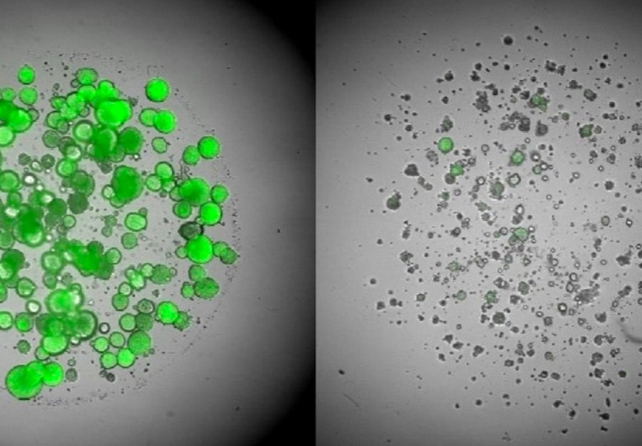 Triple-negative breast cancer cells before treatment (left) and after (right). (The University of Adelaide)
Triple-negative breast cancer cells before treatment (left) and after (right). (The University of Adelaide)CDDD11-8 even has a possibility of working on humans. Testing its effects on patient-derived breast cancer tissue and three-dimensional organoids, the team found encouraging signs of success without toxic side effects on healthy cells.
This is probably because healthy cells are not as dependent on CDK9 activity as some cancerous cells, the authors explain.
"While this drug is showing promise as a potential treatment for triple negative breast cancer, it needs further development before it can progress to human trials," concludes Hickey.
"I'm hopeful this will happen within the next five years, if not sooner."
The study was published in Oncogene.

 11 months ago
79
11 months ago
79 

